Osteoporosis: Why It Occurs & What to Do About It
April 12, 2022
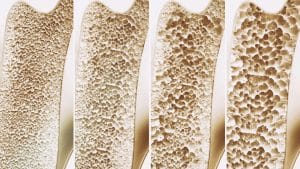
Throughout our lifetimes, our bones are constantly developing and strengthening. Our bones are at their most dense when we are in our early 20s, which is called peak bone mass. But as we grow older, bone loss may outpace the growth of new bone. Certain life events, such as going through cancer treatments, may also impact our bone health.
Symptoms & Risk Factors for Osteoporosis
There typically are no symptoms in the early stages of bone loss. Once your bones are weakened by osteoporosis, you might have signs and symptoms such as back pain caused by a fractured or collapsed vertebra; loss of height over time; stooped posture; or a bone that breaks much more easily than expected.
The most common fractures associated with osteoporosis occur at the hip, spine, and wrist. The likelihood of these fractures occurring, particularly at the hip and spine, increases with age in both women and men.
Several factors can increase the likelihood of developing osteoporosis, including your age, race, lifestyle choices, and medical conditions and treatments.
- Your sex & sex hormones. Women are much more likely to develop osteoporosis than men. Lowered sex hormone levels tend to weaken bone, and the reduction of estrogen levels in women at menopause is one of the strongest risk factors for developing osteoporosis.
- Age. The older you get, the greater your risk of osteoporosis. This is true for men and women.
- Race. You’re at greatest risk of developing osteoporosis if you’re white or of Asian descent.
- Family history. Having a parent or sibling with osteoporosis puts you at greater risk.
- Body frame size. Men and women who have small body frames tend to have a higher risk because they might have less bone mass to draw from as they age.
- Low calcium intake. A lifelong lack of calcium plays a role in the development of osteoporosis. Low calcium intake contributes to diminished bone density, early bone loss, and an increased risk of fractures.
- Steroids & other medications. Long-term use of oral or injected corticosteroid medications, such as prednisone and cortisone, interferes with the bone-rebuilding process.
- Other medical problems. The risk of osteoporosis is higher in people who have certain medical problems, such as celiac disease; inflammatory bowel disease; kidney or liver disease; cancer; lupus, multiple myeloma; and rheumatoid arthritis.
- Sedentary lifestyle. People who spend a lot of time sitting have a higher risk of osteoporosis than do those who are more active.
- Excessive alcohol consumption. Regular consumption of more than two alcoholic drinks a day increases your risk of osteoporosis.
- Tobacco use. The exact role tobacco plays in osteoporosis isn’t clear, but it has been shown that tobacco use contributes to weak bones.
- Eating disorders. For those who have severely restricted food intake and are underweight, bones may be weaker in both men and women.
It is possible to take steps to prevent and treat osteoporosis. It’s now a largely treatable condition with a combination of lifestyle changes and appropriate medical treatment.
- Calcium. Calcium is thought to be particularly important. Men and women between the ages of 18 and 50 need 1,000 milligrams of calcium a day. This daily amount increases to 1,200 milligrams when women turn 50 and men turn 70. If you don’t think you get enough calcium from your diet, you may want to consider calcium supplements. However, too much calcium has been linked to kidney stones, and some experts suggest that too much calcium, especially in supplements, can increase the risk of heart disease. Always consult your doctor about this.
- Vitamin D. Vitamin D improves your body’s ability to absorb calcium and improves bone health in other ways. We can get some of our vitamin D from sunlight, but supplements may be necessary for various reasons.
- Exercise. Exercise can help you build strong bones and slow bone loss. Exercise will benefit your bones no matter when you start, but you’ll gain the most benefits if you start exercising regularly when you’re young and continue to exercise throughout your life.
Cancer Treatment & Osteoporosis
Cancer patients can become vulnerable to osteoporosis and bone fractures as a result of both tumors and the treatment to eliminate them. Although primary bone cancer that originates in the bones is rare, other forms of cancer often metastasize into the bones. Women are naturally at a higher risk for osteoporosis due to a number of factors like decreased estrogen production after menopause. Drug therapies for breast cancer may involve suppressing estrogen levels to inhibit tumor growth, which puts the bones at risk for fractures.
Similarly, men in treatment for prostate cancer may receive hormone therapy that can weaken bone density as well. Along with the other side effects that come with cancer treatment, cancer patients with weak bones to begin with can be more susceptible to accidents and falls, have more pain, and a lower quality of life. Taking precautions to treat osteoporosis before the symptoms accelerate can help to minimize its effects.
Kyphoplasty, also known as osteoporosis-fracture treatment, is a minimally invasive procedure used to repair bone fractures and collapsed vertebrae in the spine due to osteoporosis. Using an inflated balloon to open a cavity in the bone, the surgeon then fills the space with a bone-cement compound made of polymethyl methacrylate, or “PMMA,” to strengthen the bone and act as a type of cast. The entire procedure, performed on an outpatient basis at our clinic in Birmingham, lasts around 45 minutes with a short, one-hour recovery period.
Remember that while osteoporosis itself isn’t painful, it does lead to fractures and other painful problems, usually becoming more severe with age. It’s not an inevitable part of growing older though, and there are a variety of treatment options we can explore to help you find relief. Let your doctor at Southside Pain Specialists know if you think you may be exhibiting signs of osteoporosis, and we will help find ways to manage it.
Start your pain management journey by scheduling an appointment at Southside Pain Specialists
With highly specialized training and a multitude of pain relief options, Southside Pain Specialists follow the standards of the American Society of Interventional Pain Physicians, The American Board of Pain Medicine, and the International Spinal Injection Society. We work hard to provide patients with comprehensive, caring pain relief when they need it most. Check out our website or contact us today at 205.332.3155 to learn more.
